The Medicine behind the Miracle: What is ECMO?
Recently, the incredible story of a lost hiker found on Mt. Rainier, transported to Harborview Medical Center, and treated by a team of UW physicians and nurses where he was “brought back to life” has been circulating locally, nationally, and internationally.
Mainly, the world has been fascinated by the fact that this man—whose heart stopped for 45 minutes—was resuscitated thanks to a little-known (to the layperson) technology called Extracorporeal Membrane Oxygenation, or ECMO.
These news articles have provided a sensational account of the rescue efforts, but little has been done to explain exactly what this life saving technology called ECMO is, the teams that make it possible, and its implications in the world of medicine.
What is ECMO?
ECMO stands for Extracorporeal Membrane Oxygenation, and another name for it is ECLS or Extracorporeal Life Support. Essentially, ECMO can be used for bypass of the heart, the lungs, or both if a patient is extremely sick. ECMO is the most advanced form of artificial life support available and it borrows on technology that's been used for decades in cardiothoracic surgery called cardiopulmonary bypass.
How does ECMO work?
When someone is being treated using ECMO, blood is drained out of the patient's large veins where it is directed through a pump and into an artificial lung where oxygen is moved into the blood and CO2 is removed from the blood. This oxygenated blood is then pumped back into the patient's body. The oxygenated blood is pumped back into the body in one of two ways.
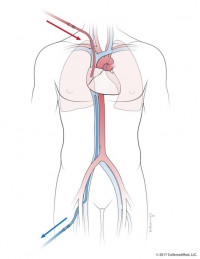
veno-venous ECMO or VV ECMO
One is through the venous system, which makes it bypass the lungs. This form of ECMO, known as veno-venous ECMO or VV ECMO for short, is used for severe lung disease, including some patients who are sick with COVID-19.
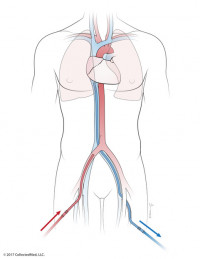
veno-arterial ECMO or VA ECMO
Another option is for the blood to be injected back into the arterial system, which means that you're bypassing both the heart and the lungs. This form of ECMO, called veno-arterial ECMO or VA ECMO for short, can support patients who are having both heart and lung failure.
VA ECMO is what is used for patients who are in cardiac arrest, also called ECPR or Extracorporeal Cardiopulmonary Resuscitation. When someone's heart isn't beating, doctors can bypass their native heart and lungs with this machine until they are able to restart their native heart, put in a device, or transplant their heart.
How long can someone be supported by ECMO?
For the type of ECMO that supports both your heart and the lungs, VA ECMO, generally patients are not on this for longer than about a week. Generally, by that point, doctors are considering more definitive options or hoping for recovery.
For the other kind of ECMO where doctors are only bypassing the lungs, VV ECMO, is a little bit trickier because doctors are waiting for the lungs to recover, and it can take some time. Two weeks is the average duration that someone is on VV ECMO.
Doctors note that there aren't many problems that ECMO itself can fix; it usually buys them time to either figure out what the problem is and try to fix it, or it acts as a bridge to the patient recovering or a more durable solution like another device or an organ transplant. Unfortunately, doctors cannot keep a patient on this device for an indefinite amount of time. It is a temporary device and it only provides that bridge to something else.
Is ECMO a recent development?
ECMO has been around in some form for quite a long time. The earliest case of cardiopulmonary bypass, which is the technique from which ECMO is derived, was in the 1950’s. Modern ECMO evolved out of that practice, but certainly over the past 10 to 15 years, ECMO technology has gotten better to the point where it is now usable in many more situations. Most recently, doctors have gained experience using ECMO for selected patients with COVID-19; UW Medicine has been a leader in the region.
Why “brought back from the dead” is not exactly the right terminology to use in this case.
When trying to explain what cardiac arrest means, it can be confusing when using different kinds of words. So, when doctors use language like “the patient died” or “was dead for 45 minutes,” they are referring to the native heart not working, and you can't be alive if your native heart does not work. If your heart doesn't beat, then you will eventually be declared dead because you need a beating heart to stay alive. What doctors mean by saying this is that the patient's heart was not beating, and they were trying to do CPR or chest compressions to help it beat because it won't do so on its own until they can find a way to bypass it and restore blood flow to organs by using VA ECMO.
So, while the word dead has a certain personality to it, physicians don't want to confuse anyone by insinuating that they can bring someone, who has been declared legally dead, “back from the dead.” These physicians are taking a patient whose heart has stopped, who needs that heart to beat in order to stay alive, and trying to buy more time to restart their heart.
What kind of system-wide coordination was necessary to treat this patient using ECMO?
ECMO is a complex form of artificial life support, but the technology itself is only one piece of the puzzle. ECMO is a “team sport” and would not be possible without many different highly trained people working in very well-defined roles to make this possible, including all of the support staff for all of the devices and for the hospital and the facilities.
In general, there is an immense amount of coordination that goes into a well-functioning ECMO program, especially within our university system. The University of Washington Medical Center at Montlake and Harborview Medical Center have both been extremely supportive of each other; these two campuses work together with ECMO programs to support patients. ECMO within UW Medicine consists of two programs at the different hospitals, but they are comprehensively integrated. It is a program that works together very seamlessly and moves patients between the hospitals based on their needs.
In the case of the hiker, there were a number of search and rescue teams involved, including the National Park Service and several of the local and regional volunteer search and rescue teams. The US Navy dispatched a search and rescue helicopter who ultimately located the patient and flew the patient to Harborview Medical Center, and the Navy personnel accompanied the patient into the emergency department. In most cases of patient transport, UW ECMO partners with Airlift Northwest to retrieve patients throughout the Pacific Northwest region, as well as Alaska, Montana, and Idaho.
There was a large team in the Harborview emergency department that included UW EM Drs. Ashley Amick and Amy McManus, as well as other resident doctors, nurses, and respiratory therapists who provided initial care for the patient in the emergency department. The trauma surgery team led by Drs. Eric Van Eaten and Katie Iverson were also present because there was concern that this patient initially had a major injury.
UW EM and Critical Care Drs. Jenelle Badulak and Nick Johnson were part of the ECMO team that responded initially and assisted with ECMO. Dr. Deepika Nehra was the ECMO doctor that cared for him in the hospital. The anesthesia and vascular surgery teams also helped care for the patient who needed some operating room procedures early and later on. There is a team in the trauma surgical ICU who cared for the patient, including Dr. Sam Arbabi, the surgeon and intensive care doctor, and Whitney Holen, one of the nurses that was quoted in some news articles, but there are many others; they are all the other people that rarely get recognized in situations like this, but are so critical to the team.
Staff from clinical engineering help keep these devices up and running. There is also the team from environmental services who keep the rooms safe and clean, especially during this pandemic, and many, many others.
Overall, it was many dozens of people who contributed to this great outcome, who all work together perfectly synchronously.
EM and Critical Care Drs. Jenelle Badulak and Nick Johnson contributed to this story.