Faculty and residents present at 2024 SAEM Conference
A broad range of faculty members and residents from the University of Washington Department of Emergency Medicine presented at the 2024 SAEM Annual Conference. Below are the objectives and summaries of their presentations.
Didactic
Drs. Dave Lu, Arvin Akhavan, Haley Egan (PGY-2)
Socks for Cold Feet: Insights From Emergency Medicine‐Bound Medical Students Who Ultimately Chose Another Path (CDEM and RAMS Sponsored)
- The 2023 SAEM Workforce Committee spearheaded a qualitative study investigating reasons why some medical students chose, or ultimately not chose, a career in EM. This study, entitled “Cold Feet,” explored the views of graduating medical students from across the country who self-identified as having seriously considered EM but ultimately chose another specialty. Results from this qualitative study were eye-opening, and included insights on the benefits of an EM career that initially attracted these students as well as the perceived negatives of an EM career that swayed these students to choose another specialty. In this didactic, they briefly presented qualitative data from this study, followed by a panel discussion with study investigators and GME and UME leaders on lessons learned and on actionable strategies to encourage student interest in and applications to EM.
Dr. Herbie Duber
Don't Just Collect Data, Use It! Transforming Care With Social Drivers of Health Data (ADIEM, AAAEM, and Social EM and Population Health Interest Group Sponsored)
- Social drivers of health (SDOH) are powerful mediators of poor health outcomes, increased Emergency Department (ED) utilization and higher healthcare costs. The ED is uniquely positioned to bring SDOH screening to the bedside and develop effective interventions. CMS and Medicaid funding opportunities and priorities provide an important opportunity to implement novel SDOH screening and intervention projects. The key lesson from this didactic session was to recognize the untapped potential of SDOH data in clinical medicine, moving beyond its role in uncovering the broader determinants of health issues and risk adjustment to building targeted referral and intervention programs. The panelists, each with content expertise on specific populations (i.e., pediatric EM, HIV/syphilis, population health, and health policy) from various institutions, shed light on how certain social factors can be applied in clinical management. This session concluded by underscoring the need for policy and advocacy to highlight the pressing need for active research in this area.
Dr. Amber Sabbatini
So You're Thinking About an R01: Roundtable Discussion on Transitioning to an Independent Investigator (Research Committee Sponsored)
- In the past decade, there has been a significant expansion of emergency medicine (EM) focused research training programs and a growing cadre of academic emergency physicians who are pursing research careers. While an increasing number of junior faculty are successfully competing for career development and other training awards, EM still ranks near the bottom of medical specialties in success in obtaining independent federal funding. There are less than 10 NIH R01s awarded annually to emergency physicians across the US, which comprise less than 2% of all R01 grants. Only a third of individuals who obtained a mentored award will successfully transition to R01 or equivalent funding, with these awards being concentrated among a handful of institutions with exceptional resources for research. Multiple challenges exist that limit retention of talented physician-scientists and there is a substantial need to provide support for individuals who are in this mid-career stage. This moderated roundtable discussion identified several challenges and considerations for researchers wishing to pursue R01 or equivalent funding, and potential solutions for these challenges, including differences between project and mentored grants, timing, FTE support and bridge funding, team development and staffing, how to negotiate shifting relationships with mentors, among others.
Dr. Marie Vrablik
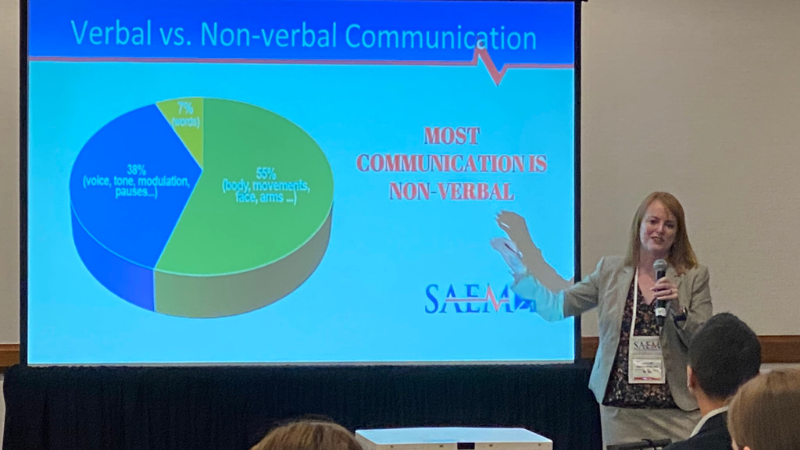
Current Best Practices for Managing Agitation and Workplace Violence: Mastering Coordinated Responses, De‐escalation Strategies, and Medication Proficiency (ADIEM and Behavioral and Psychological Interest Group Sponsored)
- Emergency Departments (EDs) are seeing a rising number of visits for behavioral emergencies. As a result, providers and health workers face increasing safety threats from workplace violence while treating episodes of acute agitation. Unfortunately, the literature has shown that emergency physicians often lack formal training in agitation management despite reports of high violence exposure rates. Expert recommendations exist regarding verbal de-escalation and physical conditions when engaging this population, but implementation can be challenging in an innately chaotic work environment and during high patient census. Recent work by our team has also called to light potential implicit bias and racial differences during agitation care, which is especially important given current societal concerns regarding police reform and interface with potentially agitated individuals prior to arrival in the ED. This session aimed to shed light on a rising but understudied clinical issue and provide evidence-based strategies to improve safety for emergency physicians and trainees while caring for this vulnerable patient population.
Dr. Fiona Gallahue
What to Expect When You're Expecting Unionization
- In recent years, the landscape of graduate medical education has witnessed a growing trend in house staff unionization. This phenomenon has posed unique challenges and opportunities for program directors across the country. To shed light on this topic, they presented their experiences and lessons learned as program directors in recently unionized programs. This peer-led discussion aimed to help program leaders understand the logistics of house staff unionization, its impact on program dynamics, and strategies to foster positive relationships within this evolving landscape.
Dr. Nathan White
The Bleeding Edge: An Update on Hemorrhage Control Therapies in Trauma
- Management of hemorrhage in trauma patients is a critical skill in the practice of emergency medicine. Recent advances in the area have deepened our understanding of the complexity of hemorrhage and given us more powerful tools to use in its treatment with many more on the horizon. These advances include a more complete understanding of the contributions of coagulopathy and endotheliopathy and the complex interplay with traumatic brain injury. We have also learned about the effectiveness of novel transfusion and blood product resuscitation strategies and mechanical hemostatic methods such as complete and partial REBOA (resuscitative endovascular balloon occlusion of the aorta) and SAAP (selective aortic arch perfusion) to support perfusion of vital organs. This session was a discussion with experts in the field, providing updates on recent advances in the understanding and management of traumatic hemorrhage, as well as previews of upcoming breakthroughs.
Trauma
Dr. Alex St. John
N‐Acetylcysteine Improves Renal Microvascular Blood Flow in a Rat Model of Polytrauma
- Microvascular blood flow (MBF) is an important measure of organ perfusion in critical illness. MBF derangement after trauma is associated with organ dysfunction, coagulopathy, and death. The mechanisms causing this derangement are not well-defined, but systemic microvascular thrombosis has been implicated as a possible cause. Severe trauma leads to oxidative conditions in the blood, and oxidative modifications of several key hemostatic proteins can promote off-target thrombus formation. We hypothesized that the antioxidant agent N-acetylcysteine (NAC) could reverse these effects and improve renal MBF after injury in a rat model. NAC improved renal MBF in this rat model of polytrauma. This confirms that oxidative stress plays a role in MBF impairment after trauma and identifies an early possible therapeutic target for improving MBF. However, NAC is a nonspecific antioxidant, and further investigation is needed to define the pathways involved.
Dr. Rachel Ann Nolan (PGY-3)
Balanced Resuscitation of Polytrauma Using a Multifunctional Resuscitation Cocktail in a Swine Model
- Trauma casualties often face the dual challenge of traumatic brain injury (TBI) and hemorrhagic shock. Combat medics encounter the difficult task of managing these co-occurring conditions with conflicting resuscitation goals. Current strategies, including permissive hypotension and aggressive volume expansion, present risks of secondary brain injury and increased hemorrhage. This study explores a multi-functional resuscitation cocktail aiming to minimize blood loss and prevent secondary injuries.
- Conclusion: The DCR cocktail, comprising Hextend, vasopressin, and fibrinogen concentrate, enhanced survival in polytrauma settings with dilutional coagulopathy. It also showed potential advantages in brain protection post-TBI, suggesting that the DCR cocktail may offer benefits in coagulopathy, cerebral resuscitation, and prevention of secondary injury in larger-scale studies.
Dr. Nathan Dow (PGY-1)
Fibrin Degradation Products: Potential Therapeutic Targets in Trauma-Induced Coagulopathy
- Trauma is a leading cause of death worldwide and the leading cause of death in the United States for young people and most early preventable deaths in this setting are due to uncontrolled hemorrhage. Trauma-induced coagulopathy (TIC) complicates post-injury care and is associated with an increased risk of morbidity and mortality, but the underlying mechanisms that drive TIC are poorly understood. Fibrin degradation products (FDPs) are often elevated in critical illness including massive trauma and are recognized as a risk factor for coagulopathy. This work aims to investigate the role of individual FDPs in anticoagulation, clot formation, and fibrinolysis.
- Conclusion: FDPs, particularly fragments D and D-Dimer, enhance fibrinolysis by increasing plasmin activity. Fragment X affects clot formation primarily by disrupting fibrin polymerization during clot formation. Traditionally, tranexamic acid (TXA) has been a key therapeutic in TIC by inhibiting the conversion of plasminogen to plasmin. This work suggests that pro-thrombolytic FDPs may also be a therapeutic target. Further work, both in samples from trauma patients and in whole blood, is needed to further characterize the impact of individual FDPs on clotting parameters and plasmin activity after injury.
Sarah Stucky (Research Study Coordinator)
Extracellular Actin Potentiates Platelet Aggregation Through Collagen Activation Pathway
- Tissue damage from severe trauma can lead to massive release of the cytoskeletal protein actin into the blood. Extracellular actin has complex effects on blood clotting, and excessive actin release is associated with platelet dysfunction after severe trauma. This implicates extracellular actin as a possible contributor to the changes in coagulation and microcirculation seen after trauma. However, actin’s specific effect on platelets and the pathways involved have not been directly tested and remain unknown. With these experiments, we sought to test and quantify this effect and begin to identify possible mechanistic pathways involved.
- Conclusion: The addition of exogenous muscle actin increases the platelet aggregation response, and this was noted through the collagen but not the ADP activation pathway. This suggests that actin release after injury could cause an overactivation response by platelets and contribute to the derangement of microvascular blood flow. The mechanism by which actin potentiates this activation pathway requires further characterization.
International Emergency Medicine
Samuel Lewis (PGY-2)
Association Between Retention in HIV Care and Mental Health Among Refugees in Uganda (GEMA Sponsored)
- Refugees living in Uganda confront significant barriers to engaging in HIV care and face an increased risk of mental health disorders due to experiences of trauma, violence, and displacement. The relationship between mental health disorders and engagement in HIV care among refugees is poorly understood. The objectives of this study were to describe the prevalence of those screening in for mental health disorders, assess retention in HIV care, and evaluate the association between mental health disorders and retention in HIV care among individuals newly diagnosed with HIV in a refugee settlement in Uganda.
- Conclusion: In a majority refugee cohort of individuals newly diagnosed with HIV, there was a high mental health disorder burden (63% screening positive for ≥1 disorder) and low levels of retention in HIV care ( < 40% at one year) but no significant association between the two. Further research is needed to better understand mental health, HIV care engagement, and their interplay in this humanitarian crisis affected population.
Critical Care/Resuscitation
Jordan Sheehan (PGY-3)
A Pathway for Safe Extubation of Selected Patients in the Emergency Department
- Emergency department (ED) boarding of critically ill patients is increasing. Extubation of highly selected mechanically ventilated patients in the ED warrants exploration as it may improve resource utilization and patient comfort. The objective of this study is to investigate the safety and efficacy of an extubation pathway in the ED.
- Conclusion: This pilot study demonstrates the feasibility and safety of an ED extubation guideline for highly selected patients. Within a small cohort, we noted zero unplanned re-intubations and relatively short hospital LOS. Future work includes expanding this pilot to include more patients and comparing resource utilization, including ventilator days and hospital LOS, to a matched cohort of patients not extubated in the ED.
Emergency Medical Services
Dr. Lakota Cheek (PGY-4)
Are Rurality or Deprivation Associated With Variation in Emergency Medical Services Care in Patients With Myocardial Infarction?
- Large variations in outcome for patients with ST-elevation myocardial infarction (STEMI) exist. We assessed if rurality or area deprivation of the neighborhood where STEMI occurred explained variation in EMS process and outcomes using a contemporary national registry.
- Conclusion: Rurality and deprivation were associated with variation in EMS process but not hospital-based outcome after STEMI. Strategies are needed to reduce disparities in EMS care. EMS data collection can be used to identify opportunities to improve emergency cardiac care.
Innovations
Nico Fesser (PGY-2)
Medicolegal Day Curriculum Provides a Realistic and Novel Educational Experience for Residents
- According to a recent study released by the AMA, one-third of physicians will be sued during their career, with other sources citing even higher percentages. Emergency Medicine (“EM”) physicians are among the most likely to be sued. The importance of medicolegal education has been recognized for more than 30 years, however, there is no standard ACGME requirement for residency programs to include medicolegal education in their curriculum. The University of Washington Department of Emergency Medicine (“UWEM”) developed a novel curriculum which aims to provide medicolegal education to residents, the goals of which are to educate residents on: medicolegal issues commonly faced in the Emergency Department, common allegations of medical malpractice lawsuits, basic elements of a medical malpractice lawsuit, the deposition process, physician errors that may lead to lawsuits, clinical practices that minimizes one’s liability, and common legal terms.
- Outcomes: The outcome included an overwhelming response from residents that it was one of the top, if not top, rated educational experiences of their residency. They left the day with a real-life experience of being deposed, lessening the anxiety of such in the future, and practice ways to better protect themselves from being sued in the future.
Infectious Diseases
Dr. Chris Buresh
Syphilis Screening in the Emergency Department in Seattle, Washington
- Syphilis infections have surged in King County, WA since 2019, causing an epidemic and increased stillbirths. Many infected individuals, especially those from non-traditional care-seeking populations, are presenting in the Emergency Department (ED). This descriptive analysis examines people with a new diagnosis of syphilis, their diagnostic and treatment locations, emphasizing the ED's role in tackling this epidemic.
- Conclusion: Data reveals shifting syphilis patterns, notably increased cases among 30-44-year-olds from racial minorities, with a substantial decline among MSM. Rising infection rates among men having sex with women and women of reproductive age are evident, along with an increase among individuals facing housing instability. Continuing to expand testing for syphilis in the ED is vital to this effort. Increasing coordination with departments of public health, as well as identifying and overcoming barriers to same-day treatment is critical.
Social Emergency Medicine
Dr. Callan Fockele
Improving Postoverdose Care: First Responder Perceptions of Harm Reduction in the Field
- Recent policy changes in Washington State present a unique opportunity to pair evidence-based interventions with first responder services to combat increasing opioid overdoses. However, little is known about how these interventions should be implemented. In partnership with the Research with Expert Advisors on Drug Use (READU) team, a group of academically trained and community-trained researchers with lived and living experience of substance use, this study examined facilitators and barriers to adopting leave-behind naloxone, field-based buprenorphine initiation, and HIV and HCV testing for first responder programs.
- Conclusion: There was widespread support for the distribution of leave-behind naloxone, although funding was identified as a barrier. These results have informed local EMS strategic planning, which will inform rollout of process improvements in King County. Future work should evaluate the impact of these interventions on the health of overdose survivors.
Ultrasound
Elsa Lindgren (PGY-3)
Drainage of Nontraumatic Pericardial Effusion: Updates From a Multicenter Study (AEUS Sponsored)
- Pericardial effusion with tamponade may lead to hemodynamic compromise requiring rapid intervention. Cardiac point of care ultrasound (POCUS) has been shown to lead to earlier diagnosis and drainage of pericardial effusions at a single site. We hypothesized that POCUS performed by the emergency physician would decrease time to drainage across multiple sites.
- Conclusion: POCUS was associated with decreased time to drainage for non-traumatic pericardial effusion. POCUS patients were found to have a higher rate of tamponade, yet a higher rate of discharge by HD 7 compared to patients that did not undergo POCUS and lower rates of UIT and RRT utilization. These findings suggest that emergency physician-performed POCUS can decrease time to intervention and adverse events during hospitalization for patients with pericardial effusion.
Forums
Dr. Sue Stern
SAEM Leadership Forum
Panel: Steve Maxwell, David Wright, Susan Stern, Debra Diercks
- This forum was designed for all levels of aspiring leaders who are interested in improving their leadership skills. The session provided exposure to core leadership topics with an emphasis on experiential learning and practical application. Presenters are recognized experts with extensive leadership experience.
- As leaders rise in the ranks in academic emergency medicine, they will need to understand how faculty are compensated. Where does the money come from? How are salaries and incentive payments determined? What factors lead to salary increases, or decreases? How is salary equity achieved? How can a department provide competitive salaries that are sustainable over time? This session made sure attendees left with an understanding of how to integrate expert and peer experience to analyze common leadership challenges, how to identify ways to inject innovation into their departments and divisions, as well as strategies to succeed when pivoting a career.
Advanced EM Workshops
Dr. Doug Franzen
The Art of Writing Effective Multiple-Choice Questions
-
CDEM has created three online tests and multiple quizzes for use by students and clerkship directors. Thousands of these exams are taken annually by students on emergency medicine clerkships, but additional work is needed each year to update the tests and develop multiple versions for administration. With an emphasis on experiential learning, this session is designed for CDEM members interested in item writing and the refinement of formative and summative assessments for EM clerkships. Participants received advanced training for item writing and blueprint formulation and prepared multiple-choice items before and after the workshop, contributing directly to CDEM's comprehensive assessments used during EM clerkships.