New treatment resources rolled out as opioid overdoses increase in Washington’s adolescents
As an emergency medicine physician at UW Medicine, Dr. Chris Buresh has a front-row seat to the effects of the opioid epidemic in Washington state. While the emergency department often sees adults struggling with opioid use disorder (OUD), there’s a concerning increase in the number of adolescents dying from an overdose.
A recent study reveals that Washington state ranks 3rd among the top 15 states most affected by opioid-related deaths in adolescents. From 2020-2022, King County saw 52 deaths among 14-to-16-year-olds due to opioids. Around 40% of adolescents who die of an opioid overdose don’t have a history of drug use, according to Buresh. With fentanyl becoming more potent and available, he said it is likely they may take something without knowing the drug is present.
“We’re in this moment where more kids are dying all the time,” said Buresh. “Yet we’re living in a time where we have more tools to address this than we’ve ever had in history. The problem is there is still tremendous stigma that prevents people from seeking treatment, and there are not many providers out there willing to prescribe these life-saving medications—especially to kids.”
The main medication Buresh champions is buprenorphine, a partial opioid agonist that can be prescribed or dispensed in physician offices. It is FDA-approved to treat moderate to severe OUD by lowering the effects of withdrawal, decreasing craving, and reducing harm and overdose associated with drug use.
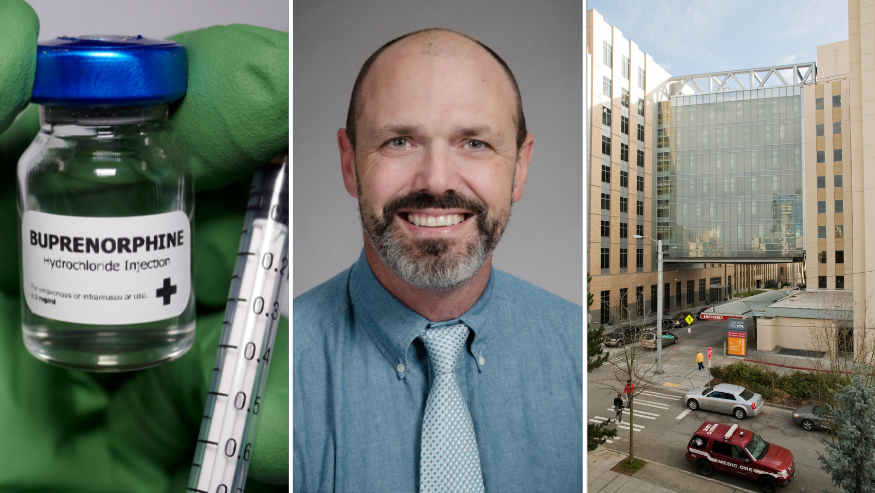
Previously, physicians had to complete additional training to administer buprenorphine, but the requirement was eliminated in 2022. Buresh thinks this could play a factor in providers not prescribing it.
“I don’t think that message that there’s no more special training got out as widely as it could have. I think people are still left with the impression that this medication is complicated or dangerous,” said Buresh. “There’s a stigma attached to it, and you are dealing with a challenging population. But the upside is when it works, you literally change somebody’s life.”
Buresh uses it off-label for adolescents he sees at Harborview Medical Center (HMC) and Seattle Children’s Hospital (SCH). The dosage is relatively low and is customized to how the patient responds. He said it's already making a difference in several teens’ lives.
“One of the first kids I put on buprenorphine was homeless and using fentanyl. One day, they decided they wanted to quit. They came in through the ED and we got the patient started with treatment. Because of that, that patient is now in college and doing well," said Buresh.
Other hospitals are taking note, according to Buresh. The work conducted at HMC has become a model for Seattle Children’s. Meanwhile, other hospitals are basing several of their protocols on the standard clinical workflow that Seattle Children’s has made.
Buresh wants to increase screening for substance abuse to get more resources like Naloxone, an overdose-reversing drug, and buprenorphine to those who need it most. Two new resources are now available to connect people of all ages to treatment.
ScalaNW is a partnership between the Washington State Health Care Authority, the UW Department of Emergency Medicine, the UW Department of Psychiatry and Behavioral Sciences, and the Addiction Drug, & Alcohol Institute. It’s a new resource for providers to improve care for patients who use opioids and other illicit drugs.
The recently launched website offers a way to connect clinicians with the information needed to understand drug use better, reduce stigma, and take ownership of treating OUD effectively. Patients can also utilize the site to find buprenorphine treatment at home and information on how to reduce their overdose risk.
Buresh, a member of the ScalaNW team, noted providers will find standardized protocols for adolescents starting on buprenorphine.
Another resource is the UW telebuprenorphine program that partners with Public Health—Seattle & King County and the UW Department of Emergency Medicine. The hotline offers on-demand treatment through a free telehealth visit. Linkage to Care Coordinators help patients find care within 72 hours of their first visit. The service is for anyone 13 years or older in King County.
Buresh noted that since adults primarily receive buprenorphine, efforts continue to determine the best dosage for adolescents. The starting dose tends to be lower in this population but may involve more tailoring after the patient starts the medicine. However, he notes it is safer than the continued use of unregulated opioids.
“We absolutely have the opportunity to intervene here. We can stop this,” said Buresh.